Female patient 48 yo came to Medic Center for a check-up .
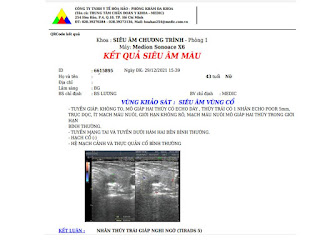
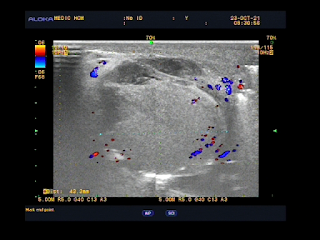
Ultrasound for thyroid incidentally detects a small nodule in left lobe that belongs TI-RADS 5 classification. Solid nodule, not well limited border, hypoechoic, non hypervascularized without calcification.
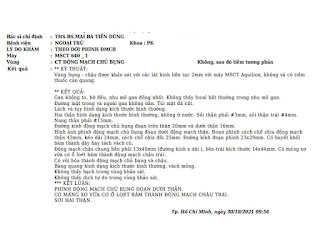
Lab data TSH usensitive 1.4ulU/mL, free T4 1.13ug/dL, Antithyroglobulin 498UI/mL, Anti Microsomal [TPOAb] 37.47UI/mL.
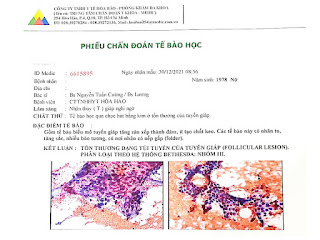
Although there is guidelines of no need to biopsy for thyroid nodule under 1 cm of diameter, a FNAC was performed.And histopathological report is a follicular lesion, BETHESDA System Group III that means a follow-up planning must be made and in some day removing small tumor will be done.