A HTA 65 year-old female with chest pain, mild apsnea and without gastroenterological symptom.
Ultrasound incidentally detects a 37x29 mm hypervascular hypoechoic mass which seems to be from the small bowel at her left abdomen.
Because of the rare incidence of small intestine (SI) tumor and in SI GIST, sonologists choose a SI polyp in differentiaziting a SI GIST.
MSCT confirms a 30x40 mm non invasive bowel wall tumor of GIST, strongly captures CE.
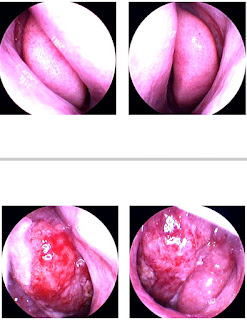
Endoscopic examination notes an exophytic jejunum tumor and open surgery removes a small intestine loop which is an adequate clearance of 5 cm upper and lower of the tumor, and performs an end-to-end anastomosis.
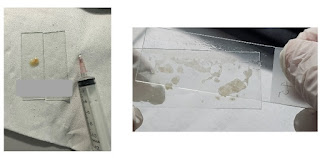
Gross specimen is a 5cm bowel intestine that exists at submucosa layer. The tumor section surface is solid, whitish with hemorrhagic ulceronecrosis.
Microscopic studies reveales spindle cells type of GIST with low mitose index.