A 70 year-old diabetic male patient with an acute abdominal pain for hours enters the emergency room of Medic Center. His prior history are 17 year known gallstone, and denies any RUQ pain or gastrointestinal troubles. He had been controlled well his glycemia. He was taken transplant coronary arterial 2 stents as 2 times of myocardial infarction for over 10 years. His EKG shows a life-rhythmic extrasystolic. WBC: 11.4H, CRP:0.4.
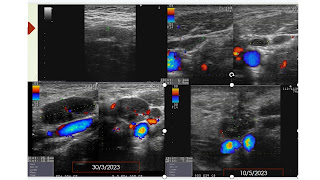
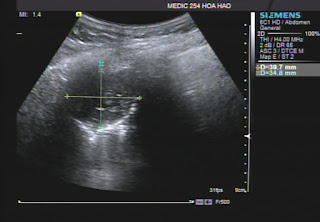
Ultrasound represents a 17 mm stone in a # 98x31 mm gallbladder with thickened wall of GB # 5-7mm. SonoMurphy sign is positive and no fluid exist around the GB.
The cholecystitis pain reduces rapidly with taken diclofenac IM, drotaverin per os after 20 minutes. But a cholecystectomy via endoscopy is planned in regarding his Clopidogrel, diabetic status and the life-rhythmic extrasystolic EKG.
Endoscopic surgery removes a 17 mm pigmented stone within a thicken gallbladder wall. The GB mucosa is partially necrosis and hemorrhage. Thicken GB wall leads endoscopic surgery cut it into small pieces for removing the gallstone and the inflamed gallbladder.
Pigmented gallstone and inflamed gallbladder in small pieces.
Endoscopic view of the inflamed gallbladder.
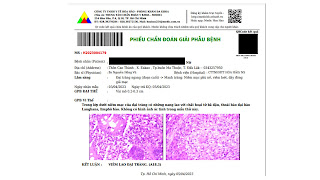
Microscopic result is a necrotic cholecystitis due to gallstone. The patient remains well and discharged in safety after 2 days in hospital.
In reviewing the gallbladder, the gross specimen of GB shows a cholecystitis image more interesting than the ultrasound view. So it makes alert when facing a painful gallstone than a silent stone of gallbladder.
Furthermore there is a proposal that should think about acute cholecystitis while seeing a gallstone in a RUQ painful patient.





.jpg)
.jpg)
.jpg)
.jpg)











.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)

.jpg)



.jpg)
.jpg)






