Total Pageviews
Saturday, 10 December 2022
CASE 659: FIBROSARCOMA of Left SCAPULAR REGION, Dr PHAN THANH HAI, Dr LE VAN THO, Dr HO CHI TRUNG, MEDIC MEDICAL CENTER, HCMC, VIETNAM
Friday, 9 December 2022
CASE 658: CYST of PROSTATE or FISTULA of INTERNAL ILIAC VESSLES, Dr PHAN THANH HAI, Dr LY VAN PHAI, Dr LE THANH LIEM, Dr HO KHANH DUC, MEDIC MEDICAL CENTER, HCMC, VIETNAM
Friday, 18 November 2022
CASE 657: MEDIASTINAL ABSCESS, Dr PHAN THANH HAI, Dr PHAN NGUYEN THIEN CHAU, Dr LE HUU LINH, MEDIC MEDICAL CENTER, HCMC, VIETNAM
A 69 year-old male patient enters Medic Center with ten days of fever, thoracic pain and trouble ingestion. He was managed as gastritis but nothing change.
MSCT represents a # 3 centimeter mass containing air which is an upper mediastinal abscess with some calcified foci inside due to a fistula of 1/3 middle part of esophagus.
Surgeon advises immediatly transferring the patient to a surgery hospital.Thursday, 10 November 2022
CASE 656: BOWEL VOLVULUS due to MESENTERIC CYST, Dr PHAN THANH HẢI, Dr TRẦN NGÂN CHÂU, MEDIC MEDICAL CENTER, HCMC, VIETNAM
Ultrasound detects a cystic mass # 17.9x11.2 centimeter from his navel to pubis, and jejunum dilatation with obstruction sign (washing machine sign). The cystic mass contents fluid and septation with vascular sign on its walls. The cause of bowel obstruction was noted by a non-dilated bowel loop at the mesenteric root with whirpool sign.
There is not bowel malrotation nor duplication cyst, so the ultrasound findings is bowel volvulus due to a mesenteric cyst.
MSCT confirms bowel volvulus due to a mesenteric cyst later.
Open surgery is done after endoscopic investigation. The cystic mass with yellowish fluid and a part of bowel are removed. Patient remains well post-op.
Saturday, 22 October 2022
CASE 655: RETROPERITONEAL GANGLIONEUROMA, Dr PHAN THANH HẢI, Dr NGUYỄN KIM HIẾU, MEDIC MEDICAL CENTER, HCMC, VIETNAM
A 19 year-old female patient with lumbago and periumbilical pain went to Medic Center for ultrasound examination for 10 days.
Abdomen ultrasound detects a calcified mass, colorless signal, close by the vertebral column on left side which is thought a TB abscess or a retroperitoneal tumor. On vertebral X-ray films there are erosions of the vertebral bodies T 11 and T 12.

MSCT confirms a tissue density mass, well limited, with calcifications inside, # 11x17x7 cm, medium contrast captured. From under the diaphragm the mass compresses left kidney and soft tissues around and erodes vertebral bodies T11, T 12. It may be a retroperitoneal neurogenic tumor.
Thursday, 20 October 2022
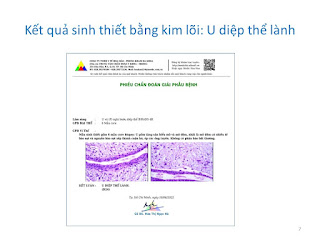
CASE 654: PHYLLODES TUMOR of the BREAST, Dr PHAN THANH HẢI, Dr JASMINE THANH XUÂN, Dr TRẦN THỊ HỒNG VÂN, MEDIC MEDICAL CENTER, HCMC, VIETNAM.




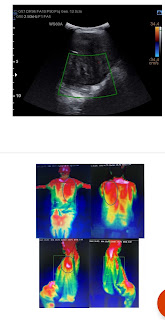





































.jpg)