A healthy 7-year-old boy on imaging examinations, including abdominal
ultrasound and computed tomography (CT):
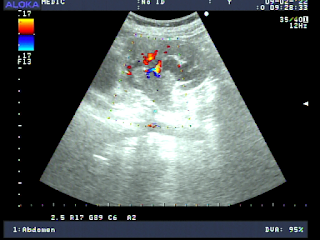
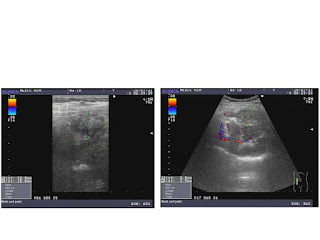
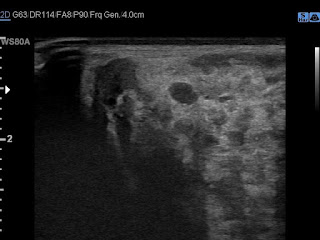
An abdominal ultrasound scan revealed a 5.3 × 5.2 cm lesion which was
homogeneous hypoechoic solid mass and its central
scar in the right lobe of the liver. It existed Doppler signals of central feeding artery in the mass on a fatty infiltrated of parenchyma of liver.
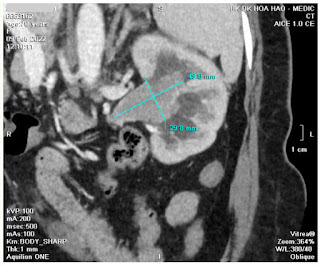
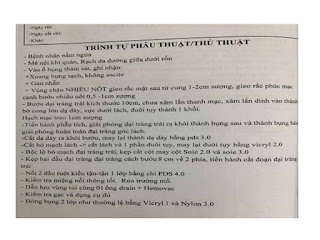
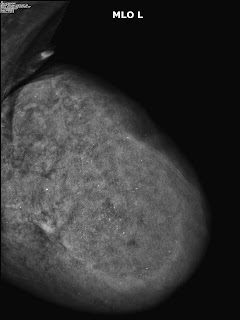
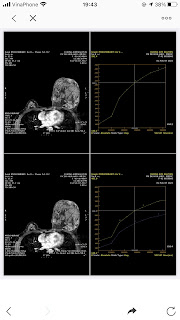
On CT of abdomen, NECT showed a 5.7 × 5.4 cm hyperdense mass in comparison to normal
liver in the right hepatic lobe, which displayed a central star-like scar in
the low-density area. On the contrast CT scan (CECT) transient, intense, and
homogeneous enhancement in the hepatic arterial phase and hyperdense to normal
liver in the venous phase. In the delayed phase, mass was in hyperdense to
liver while central scar was in hypodense density.
Laboratory testing revealed the following: alanine aminotransferase
(ALT) and aspartate aminotransferase (AST) were 30.1 U/L (normal, 3–30 U/L) and
32.3 U/L (normal, 6–25 U/L), respectively; viral serologic tests for hepatitis
B and C were negative; the alpha-fetoprotein (AFP) level was 1.6 ng/mL; and the
carbohydrate antigen 19-9 (CA 19-9) level was 7.03 U/mL.
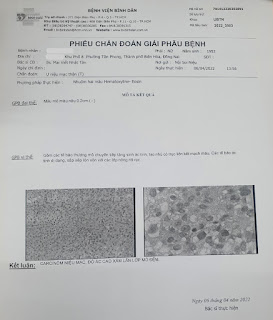
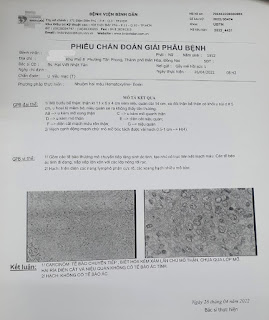
DISCUSSIONS and CONCLUSIONSPrimary tumors of the liver, including malignant and benign tumors,
constitute 1%–2% of all pediatric tumors. Focal nodular hyperplasia (FNH) is a
benign lesion of the liver which is usually found in healthy adults. However,
FNH is rare in children, and comprises only 2% of all pediatric liver tumors. It
is occasional for children suffering from FNH without symptoms. We usually use some imaging modalities (ultrasound and CT scan) to ensure the diagnosis and follow-up the FNH of liver.
References:
1. https://www.ultrasoundmedicvn.com/2017/06/case-437-liver-tumor-dr-phan-thanh-hai.html
2. https://www.ultrasoundmedicvn.com/2020/07/case-592-focal-nodular-hyperplasia-of.html