An intrahepatic pregnancy case in over 4 months could not diagnose by transvaginal ultrasound [TVS] for a 27yo patient, PARA 1001, beta HCG elevated in Kien giang province.
2 months before, on June 13, 2007, suspected an ectopic pregnancy, the patient had been removed her right ovarian tube although not finding out the gestational sac in Kien giang.
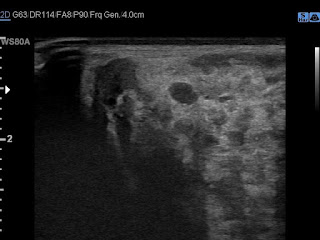
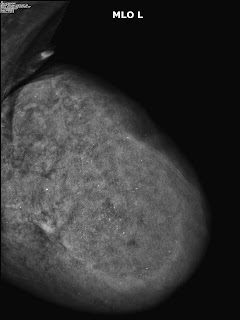
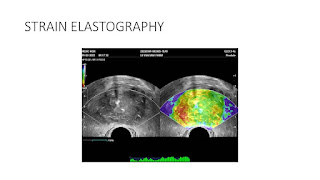
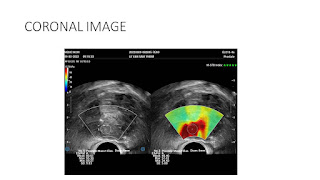
But, in 2 months later, with her RUQ pain from August 20, 2007, abdominal ultrasound at Medic Center and Tu Du hospital HCMC detected a 23 weeks fetus living in liver with positive heartbeats.
Placenta adhered largely to liver
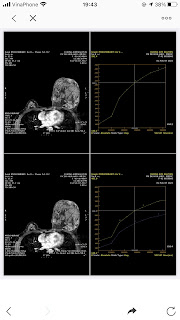
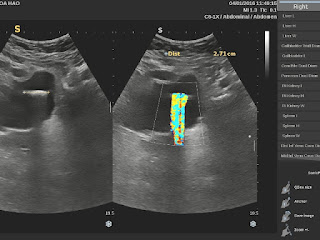
On August 28, 2007, CT confirmed hepatic pregnancy aged 23 weeks that was entirely inside right lobe of liver. MSCT Angio with CE revealed vessels of fetal bag which was from hepatic artery and placenta largely adhered to liver.
.
Ultrasound and abdominal CT in Medic Center detected a fetus # 23 weeks in the abdomen below the
right diaphragm and inside right lobe of liver. The dimensions of fetal mass were 12x15x17cm. The placenta was
47mm thick, invaded the right liver and having a vascular supply from the
right hepatic artery.
Diagnosis: great subhepatic pregnancy, indication for surgery and poor prognosis of critical case.
It would be a difficult case with high risk so Tu Du Hospital invited a surgeon from Cho Ray Hospital to perform together a surgery for the patient.
The operation removed hepatic pregnancy but placenta suddenly detached itself from liver and profuse bleeding that could not be controlled.
Surgical report:
Laparotomy on August 30, 2007, there was about 200mL of blood
flowing in the abdomen. The liver surface was smooth, but there was a lumpy mass in
segments VI, VII, and VIII which was covered by anterior surface of the liver.
Dissecting the
anterior and inferior border of the liver, a hepatic pregnancy mass was detected inside liver. The chorionic ridges of placenta penetrated deeply into the hepatic parenchyma, attaching
to 2/3 surface of the liver.
Opened the fetus bag, aspirated amniotic fluid, a dead girl fetus about
600g of weight was taken out.
Cut the umbilical cord to get the fetus and left the placenta in situ, but
the placenta detached itself from the liver, causing bleeding profusely. The surgeons had to decide to
take a part of the placenta and cut off the part of the liver that was attached to it.
This was a very complex technique and extremely difficult to
stop bleeding. Tying the blood vessels from the liver stalk, the surgeons inserted gauzes to stop the bleeding. There were transfusing 8 units of blood but it was still not controllable. About 15 minutes later, there was more bleeding from cut hepatic surface, then cardiac arrest occurred and the patient died on surgical table.
Surgical diagnosis: Subhepatic pregnancy and death due to unstoppable bleeding.
DISCUSSIONS and CONCLUSIONS
Hepatic pregnancy mass has grown (about 5 months # 20 - 23 weeks) in the diaphragmatic position and had had bleeding 2 months ago, possibly from the gestational sac.
Using only the transvaginal probe, doctors of Kien giang Province did not reveal the hepatic ectopic pregnancy and the surgeon did not find the fetus in the removed ovarian tube. Since then the fetus grew continously more 2 months and patient died due to a late ectopic pregnancy bleeding with grown fetus and placenta.
Right liver resection will be a safe solution? Currently, the technique of hemostasis of broken liver through the endovascular way is very easy to perform.
But in this case, surgeons had controlled the main hepatic artery while the blood loss from liver tissue and venous system continued bleeding due to the adhesion of placenta.
Recommendations: When diagnosing an ectopic pregnancy (GEU), an abdominal ultrasound examination should be using 2 probes together, vaginal probe and abdominal probe.
Medical treatment with MTX is safer than surgical management for early detecting ectopic pregnancy [in the abdomen, in the liver, in the spleen, ...].
The case was published in SIEU AM NGAY NAY 46, vol 2, 2007.
REFERENCES.
- PUBMED MEDLINE . Key word : hepatic ectopic pregnancy
- Williams Obstetrics..22nd Ed.. section III. Antepartum..
- Stuart H Shippey et all Diagnosis and management of Hepatic Ectopic Pregnancy, Obstet Gynecol. 2007,109 :544-6
-Prasat K.V.S. et al.. Case report Primary hepatic pregnancy, Obgyn.net/pregnancy-birth/page=/pb/articles/hepatic-pregnancy