Case 01:A 19 year-old man with fever and dyspnea for one month.
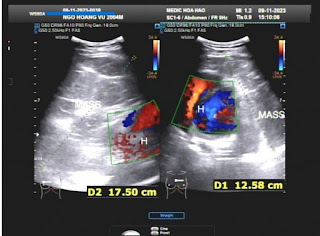
Cardiac ultrasound could not explore the anterior of the heart but no ventricular hypertrophy was noted.
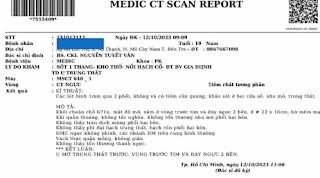
MSCT confirmed an anterior mediastinal mass.
Surgery removed the anterior mediastinal lipoma.
Chest X-RAY film post-of came back normally with no mediastinal tumor.
Mediastinal lipoma is a rare benign entity which may detect incidentally with dyspnea, difficult speaking and swallowing.
Heart shadow is large on chest X-RAY film but EKG and ultrasound are normally appearances.
MSCT detected exactly the tumor which has fatty density of 95 HU.
And it needs any further invasive technique to diagnose and management.
Reference: