A 66 year-old male patient (170 cm height, 64 kg weight) with thoracic pain was suffering from arterial hypertension [164/84 mmHg, BP 64b/min] for 3 years, and diabetes mellitus for 2 years.
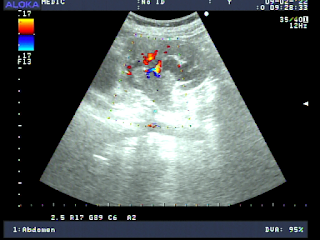
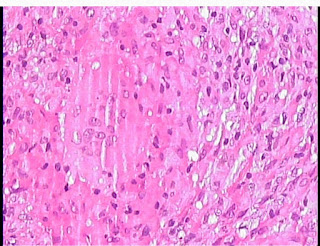
Ultrasound detected aliasing artifact from right common iliac artery [r CIA] which has been a dissection aneurysm # 34x23x20mm with 2 lumens. The peak systolic velocity (PSV) of the false lumen of right CIA was lower than the true one. It existed atheromatic plaques in the abdominal artery [AA] wall, but it [AA] was not aneurysm. A note of arterial aneurysm dissection of the right common iliac artery [r CIA] was made.
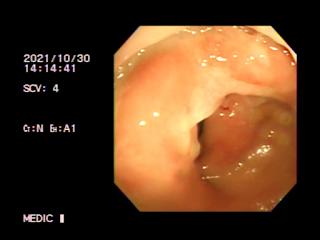
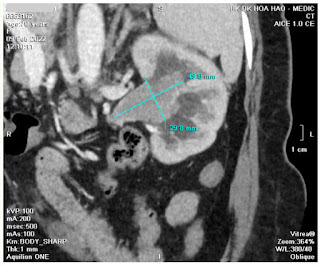
MSCT confirmed the 19x7 mm isolated right common iliac artery dissecting.
DISCUSSION and CONCLUSIONS
Isolated common iliac artery dissection is a very rare disease which is detected by chance. The possible causes included atherosclerosis, fibromuscular dysplasia, connective tissue disease, trauma and pregnancy.
It is certainly wherever to look for an arterial aneurysm in a hypertensive old patient in routine workflow not only for abdominal aorta (AAA) but also for other arteries and its branches or inside any abdominal organes.