A 64 year-old woman with fatigability in general check-up.
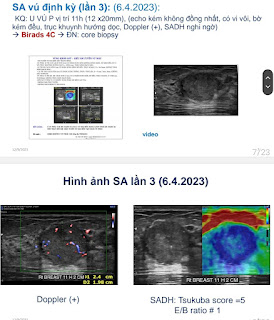
Neck ultrasound incidentally detects a right 16×11mm parathyroid tumor in right posteroinferior face of thyroid.
Laboratory findings note PTH value highly raised but not raised calcemia value. Osteogram notes her osteoporosis status with the bone fracture risk 6 times more.
Parathyroid Scan BIMI-99 Tc confirms a right parathyroid tumor.
Summary
Normocalcemic hyperparathyroidism is a newly described variant of hyperparathyroidism.
It is defined as persistently low or normal corrected or ionized serum calcium levels taken at least six months apart in the presence of elevated parathyroid hormone levels.
It may be primary or secondary. Normocalcemic secondary hyperparathyroidism is treated medically, while primary may need surgery.
….
The initial diagnostic approach for the patient is to rule out all secondary causes of hyperparathyroidism.
Normocalcemic primary hyperparathyroidism may be present in up to 17% of all cases of elevated PTH.
While usually asymptomatic, over one-third of nPHPT will progress to symptomatic bone disease or nephrolithiasis.
Familial hypocalciuric hypercalcemia needs to be ruled out. This can generally be done via a low calcium/creatinine clearance ratio.