31 year-old female patient, accountant, in
Gia Lai province. Onset 2 months with scattered body itching, no skin lesions, no fever,
no abdominal pain. A private clinic in Gia Lai, with blood tests, diagnosed
Toxocara sp infection, and gave her albendazole
800mg/day x 21 days. No itching she went down to an another private clinic in Quy Nhon province, and with another blood tests, she was diagnosed infected Cysticercosis, being treated with albendazole 800mg/day
x 10 days. Then appearing right abdominal pain, ultrasound suspected liver
damage caused by Fasciola spp. She
went to Institute of Parasitology and Entomology in Quy Nhon province and then came
to Medic Hoa Hao in Ho Chi Minh city.
Ultrasound detected right liver lesion with mixed echo,
d = 5 cm, clear border, within a few of hypoechoic nodules, and no liver tissue edema
around (Fig 1, 2). Further ultrasound detected colon wall thickness at liver region, hypoechoic, not lumen narrowing (Fig
3).
Endoscopy showed transverse colitis.
Blood tests: WBC 14,500 cells/mm3 (Neutrophil
61.9%, Eosinophil 15.8%), hsCRP 14.53 mg/L. HBsAg (-), antiHCV (-), AFP (-),
CEA (-), Fasciola sp IgG (+), stool exam (-).
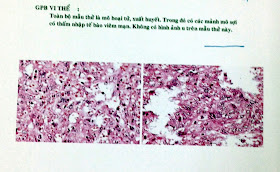
Biopsy
tissue in colon lesion was done and microscopic report was eosinophil mucosa colitis.
MSCT CE presented liver lesion d = 4x6cm and
transverse colon lesion with wall thickness d = 20mm (Fig 5, 6).
We diagnosed: liver abscess and pseudotumor colitis by
Fasciola spp (Ectopic Fascioliasis) treated with Triclabendazol 10mg/kg/day x 2 days.
Re-examination 4 weeks later, WBC 8,800 cells/mm3
(Eosinophil 2.5%), hsCRP 1.3 mg/L.
Liver lesion in ultrasound and MSCT, wall thickness d = 8mm in MSCT (Fig 8, 9).
We represented an ectopic Fascioliasis with hepatic and transverse colon lesions and an undifferential serodiagnosis. Endoscopic biopsy result helped ruling out a colon tumor. But based on ultrasound findings of liver and colon lesions which were confirmed by MSCT we could chosed a concordant diagnosis for this case.